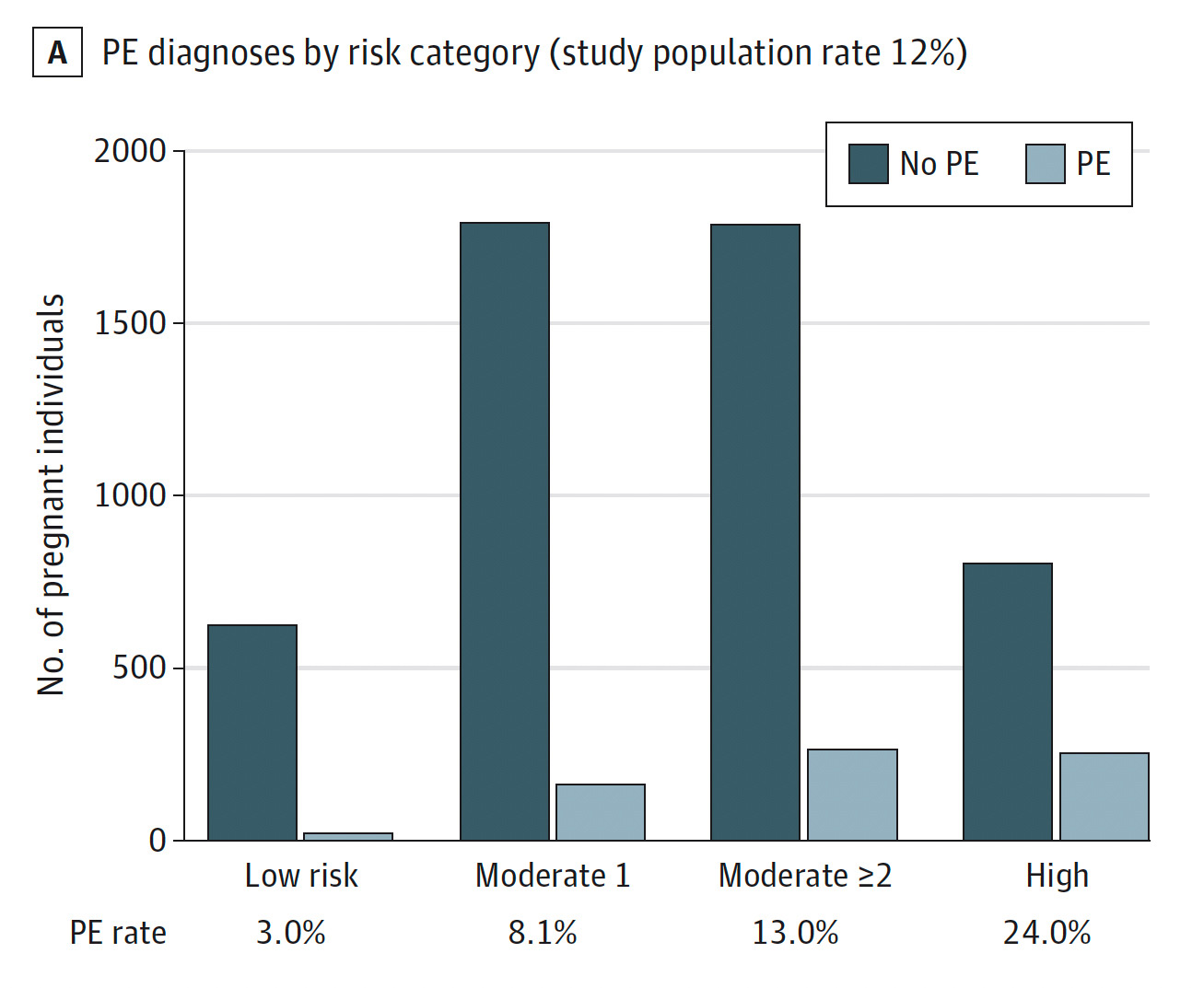
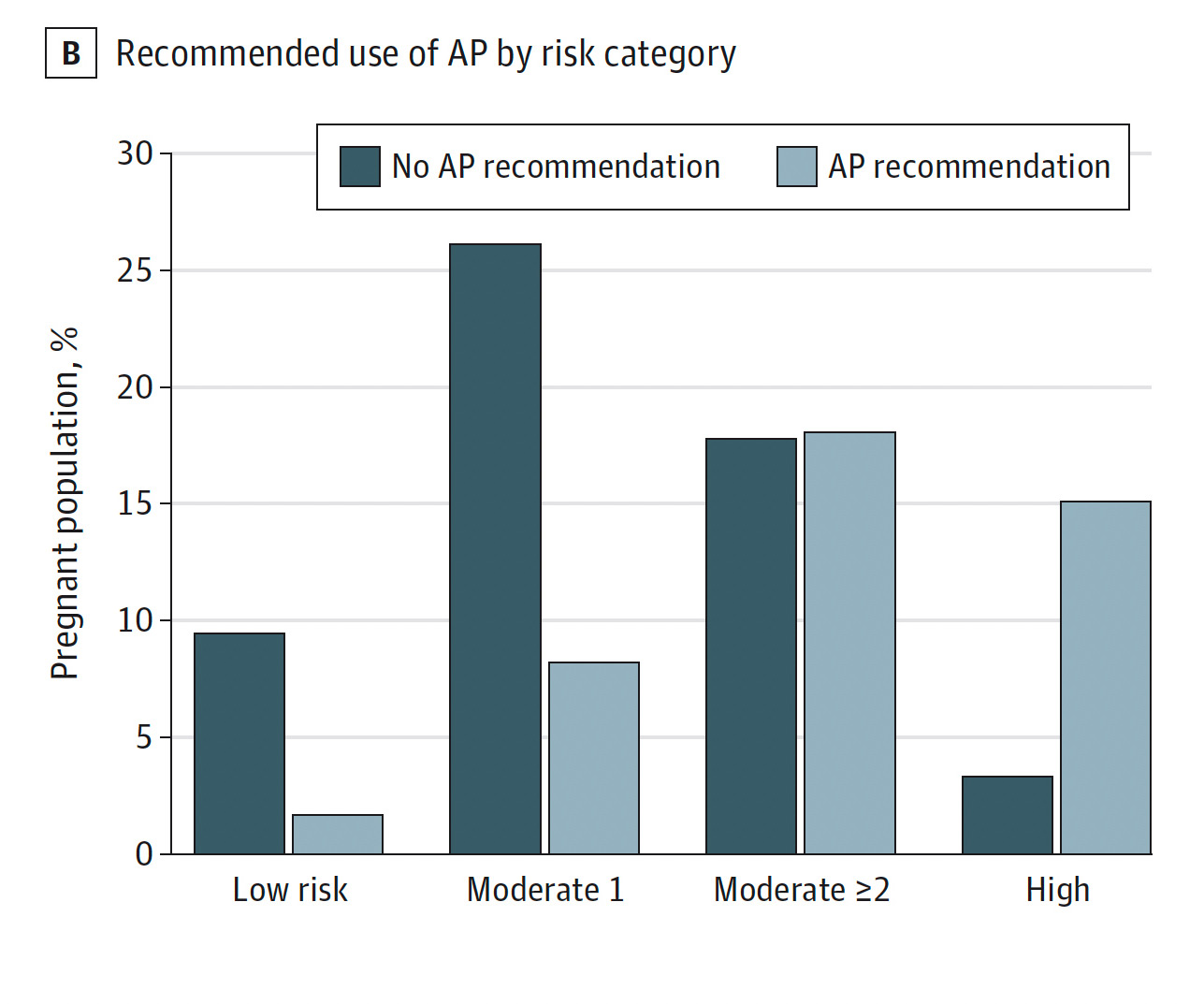
In this prospective cohort study of singleton pregnancies, 89% of the population was at increased risk of preeclampsia (either moderate or high) by USPSTF criteria. Aspirin recommendations were effectively implemented only for high and low risk categories. Moderate risk factors, in the absence of high risk factors, had little or no value for estimating the risk of developing preeclampsia, leading to nonspecific recommendation of aspirin prophylaxis in the moderate risk category.